- Home
- Cancer Immunotherapy
- CAR-T Basics
CAR-T Basics
Chimeric Antigen Receptor T-Cell Therapy (CAR T-cell)
CAR stands for chimeric antigen receptor. Chimeric Antigen Receptor T-cell (CAR T-cell) therapy is a new approach to fighting cancer using the patient’s own immune system. The immune system cells, T-cells or T-lymphocytes are normally able to identify abnormal cells, like cancer cells, and destroy them before they multiply and cause disease. Sometimes, however, T-cells have trouble detecting cancer cells.
In CAR T-cell therapy T-cells are removed from the patients’ blood and a new gene is inserted into the T-Cell to make it easier for the T-cells to fight cancer. This new gene is designed to target a specific molecule that is present on the surface of a specific type of cancer cell. Once the genetically modified CAR T-cells are infused into the patient, the cells circulate in the body looking for their specific cancer cell for which they are engineered to target. When they find the intended target, the engineered immune cells bind to the cancer cell and kill it.
How Do We Modify a Normal T-Cell into a CAR T-cell?
The white blood cells including T-Cells are separated out of the blood
An Inactive Virus is used to insert special genes into the T-Cell
The new genes cause the T-Cell to create new receptors called CAR
The new receptors on the CAR T-cell are attracted to targets on the cancer cells
These new modified T-Cells now called CAR T-cells and are then expanded to millions to create a therapeutic dose
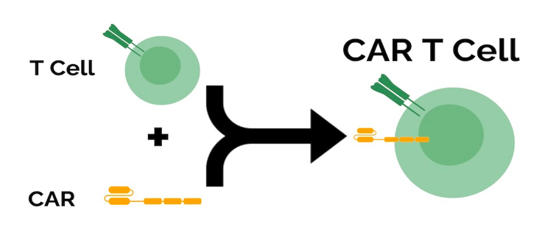
A CAR T-cell is formed when a Specific Type of Receptor called a CAR (Chimeric Antigen Receptor) is genetically inserted into the Cancer patients own T-Cells. This new and improved CAR T-cell will be better able to identify and destroy the patients’ cancer cells.
What types of Cancers can be treated with CAR T-cells?
As of 2021 the primary cancers being treated with CAR T-cell Therapy are blood cancers. CAR T-cell therapies are FDA approved to treat some kinds of lymphomas and leukemias, as well as multiple myeloma. CAR T-cells are showing promise as the most effective immunotherapy for targeting specific cancers.
Unlike most drugs, which are inanimate molecules that leave the body soon after treatment has ceased, CAR T-cells are living cells. Many versions of CAR T-cells are now also equipped to expand over time and alter their activity as well as increase their numbers after the patient’s course of treatment has ended, with the goal of providing durable benefit to patients. Some of the benefits of CAR T-cells:
The new generations of have little risk of dramatic side effects ( 2nd Generation Technology)
Generally, One Month Treatment Regiment
Overall Positive Response higher than other treatment options
Long-term Immune Boosting Effect
No Chemotherapy
Patients Own Blood Used in the Treatment
Currently, CAR T-cell therapy is typically used after other types of treatment have been tried, usually chemotherapy and the treatment failed. Most of the research has been done on CAR T-cells is with patients who have failed chemotherapy multiple times. It’s likely that many of the patients who have failed other treatments and come to try CAR T-cells would have gotten an even better response if they had tried CAR T-cells as a first option.
Basic Steps for CAR T-cell therapy are as follows:
- 50 ml of blood is collected from the patient.
- A special gene called a “Chimeric Antigen Receptor” (CAR) is added to the patient’s own T-Cells in the laboratory.
- Large numbers of the modified T-Cell now called a CAR T-cell are grown in the laboratory and given to the patient by infusion.
- These CAR T-cells will identify the patient’s cancer and destroy the cancers cells
- T-Cells have protein receptors on their surface
- T-Cells locks on to diseased cells and releases toxic chemicals through the receptor into the diseased cell
- T-Cells recruit other T-Cells to the area of the diseased cell
A reason why patients are pursuing CAR T-cell therapy is that cancer cells can disguise themselves so ordinary T-Cells cannot identify them. Cancer cells create many antigens on their surface so the T-Cells cannot “lock on”. Cancer cells can turn off the immune systems response to them by secreting certain chemical signals.
CAR T-cells can overcome Immunosuppression better than normal T-Cells. Engineered CAR T-cells are more resistant to immune suppression. CAR T-cells contain switchable receptors to circumvent immunosuppression. Regional Injections to Solid Tumors can help to minimize immunosuppression
